Overview of Medicinal Cannabis
How does medicinal cannabis work?
There are more than 100 different types of cannabinoids found in cannabis plants. Cannabinoids can also be found in the human body, these are called endocannabinoids and they affect appetite, sleep, memory, pain and inflammation.
Cannabinoids from the cannabis plant act on receptors in the brain and other parts of the body by mimicking naturally occurring endocannabinoids.
The main cannabinoids that interact with the human body are Tetrahydrocannabinol (THC) and Cannabidiol (CBD). When used separately, these cannabinoids will have varying effects on a person as each work differently.
THC may be used to reduce symptoms of nausea, vomiting, pain and muscle spasticity as well as improve sleep and appetite. In some people, THC may cause the ‘high’ generally associated with recreational cannabis use.
CBD does not cause a ‘high’ and may reduce the unwanted side effects of THC.
Research is continuing into the medicinal uses of CBD and THC combined. The combination is thought to be useful in the management of seizures and pain and may also help to reduce anxiety.
Depending on a patient’s medical condition, the doctors’ diagnosis and treatment plan will be carefully considered to ensure the medical cannabis product received contains the appropriate levels of cannabinoids for symptom management.
What are cannabinoids?
There are three general types of cannabinoids
Endocannabinoids
which are produced naturally in the human body
Phytocannabinoids
such as those present in the cannabis plant
Synthetic cannabinoids
which are man-made chemicals synthesized to mimic the activities of natural cannabinoids
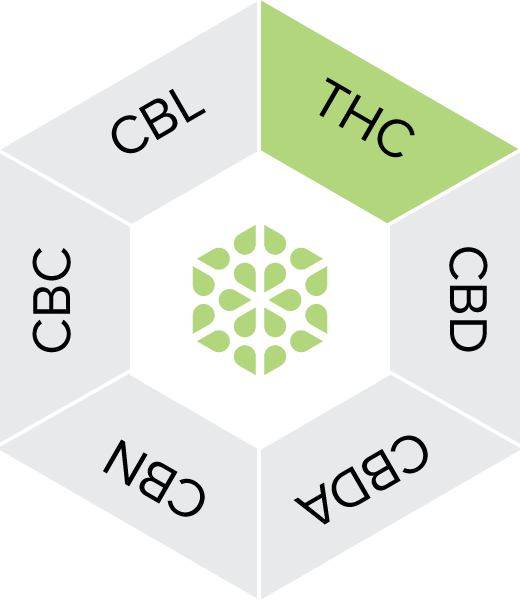
Phytocannabinoids, such as THC and CBD – the primary active cannabinoids in the cannabis plant – have been shown to imitate cannabinoids that are naturally produced in the body (called endocannabinoids), leading to a therapeutic effect in patients with certain medical conditions. Over 100 cannabinoids have been identified in the cannabis plant, many of which have been shown to have medical value.
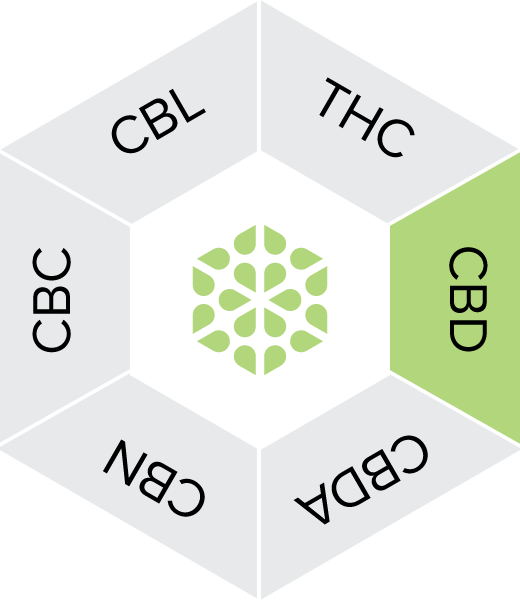
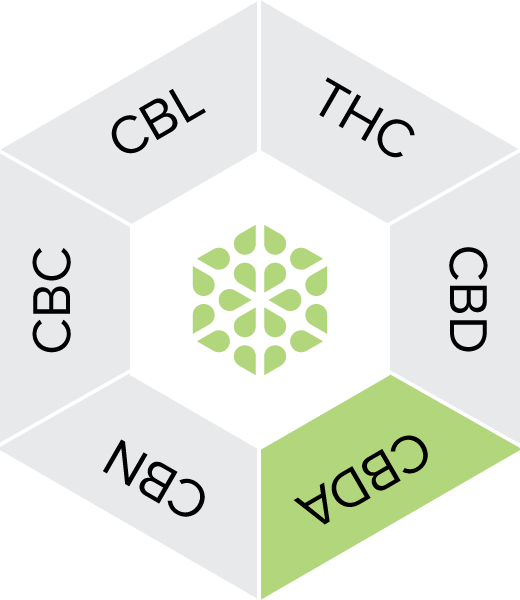
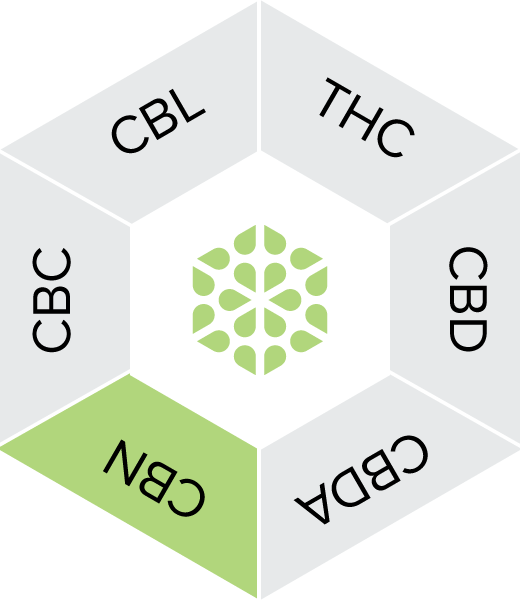
In addition to cannabinoids, the cannabis plant can contain up to 400+ additional chemical compounds, including terpenes – oils secreted in the same glands that produce cannabinoids, which are responsible for the aroma and colour of cannabis plants. Over 100 different terpenes have been identified in the cannabis plant, and every individual plant has a unique profile of terpenes and cannabinoids. The following infographic outlines the most commonly studied cannabinoids and terpenes in the cannabis plant.
THC is a neutral cannabinoid, well known for being strongly psychoactive. Some studies have shown that THC has displayed therapeutic potential for the treatment of a variety of ailments and disorders including pain and nausea.
CBD has a very wide range of pharmacological actions but minimal intoxicating effects. CBD does not bind to CB1 receptors, so it does not have the same psychoactive effect. Early evidence suggests therapeutic actions of CBD at relatively high doses (300–1500 mg) in treating epilepsy, anxiety and psychosis. Numerous clinical trials are underway for other conditions such as neuropathic pain, drug and alcohol dependence and neurodegenerative disorders.
Cannabidiolic acid (CBDA) is a cannabinoid acid naturally produced in cannabis plants, most commonly found in raw hemp and marijuana plants. CBDA is the acidic form of CBD, meaning CBDA is the precursor to CBD. CBDA does not bind directly with cannabinoid receptors. CBDA interacts with the ECS by blocking the cyclooxygenase-2 enzyme from breaking down endocannabinoids. This may allow endocannabinoids to interact with cannabinoid receptors more efficiently.
Cannabinol is a non-psychoactive cannabinoid that comes about from the oxidation of THC. It normally forms when THC is exposed to oxygen and heat. There is generally very little CBN in fresh cannabis plants.
Cannabichromene is a non-psychoative minor cannabinoid. Early research has show potential as a treatment for anxiety and stress, inflammation, and pain.
Cannabicyclol is formed when cannabichomene (CBN) is exposed to light and degrades. Very little is known about its medical properties as it appears in much smaller concentrations than other cannabinoids.
How is Medicinal Cannabis administered?
Medicinal cannabis can be administered via a variety of pathways, including but not limited to ingestion, inhalation, sublingual and topical absorption.
Oral ingestion
Many individuals choose to orally ingest their medical cannabis as oil, soft gels, or tablets. Psychoactive and physiological effects of orally consuming cannabis appear ~90 min after ingestion, reach max after 2-3 hours and last for 4-12 hours

| Absorption Pathway | Bioavailability | Onset | Peak | Duration |
|---|---|---|---|---|
| Stomach and Small Intestines | THC: 5-20% CBD: 11-19% |
90 min | 2-3 hours | 6-8 hours |
Oil
Cannabis oil is made by extracting concentrated resin, containing cannabinoids and other bioactive compounds, from cannabis flowers that have undergone thermal decarboxylation. The resin is then diluted with a pharmaceutical-grade oil to make a finished cannabis oil product that has a defined concentration of cannabinoids and terpenes.
Softgels and capsules
Softgels and capsule usually consist of cannabis resin dissolved in a carrier oil. This may provide additional convenience for patients who require additional portability.
Inhalation
Vapourising is a way to inhale the bioactive components of medical cannabis without burning the plant material. Cannabis is heated to a temperature that volatilizes, without combusting, the cannabinoids and other plant constituents, substantially reducing toxic by-products. It reduces the harms associated with smoking, is a more efficient way of extracting chemically active constituents, and reduces the loss of cannabinoids in sidestream smoke, which leads to substantial cost savings over smoking.
Ground cannabis flower is placed into a chamber where it is progressively heated past the boiling points of the bioactive compounds, but not high enough to cause combustion. The vapours are either collected in a secondary chamber or directly inhaled.
| Absorption Pathway | Bioavailability | Onset | Peak | Duration |
|---|---|---|---|---|
| Lungs | 11-45% | 0-1 min | 30 min | 1-4 hours |
Sublingual administration
Sublingual and ingested administrative methods like filmstrips, wafers, and lozenges are preferred by many medicinal cannabis patients as sublingual administration has a faster onset of effect than ingested cannabis medicines. These products are absorbed under the tongue, in the oral mucosa, bypassing the liver and reaching the blood stream in as little as 10-30 minutes.

| Absorption Pathway | Bioavailability | Onset | Peak | Duration |
|---|---|---|---|---|
| Oral Mucosal | 10-35% | 20 min – 1 hour | 30 min | 1-4 hours |
Transdermal application
Transdermal cannabis products are specially formulated to enable absorption of cannabinoids through the top layers of the skin. In many cases, transdermal medicinal cannabis products contain only CBD and are formulated to be non-psychoactive. These products are applied topically to the epidermis, where they are absorbed and interact directly with endocannabinoid receptors present in the skin.
Further evidence is required to confirm bioavailability, as well as typical onset, peak, and duration time frames for topical medicinal cannabis products.

| Absorption Pathway | Bioavailability | Onset | Peak | Duration |
|---|---|---|---|---|
| Locally at the site of application | Further studies required | Further studies required | Further studies required | Further studies required |
Evidence for the use of medicinal cannabis
Although the evidence base for medicinal use of cannabis is still developing, recent studies have shown that medicinal cannabis may have potential as a symptom management option for a broad range of medical conditions.
Most approvals under SAS-B are for the treatment of chronic non-cancer pain. This includes conditions such as arthritis, lower back pain, pain, pelvic pain, neck pain and various forms of neuropathic pain. These are typically treated with oral solutions that contain THC and sometimes additional CBD. Other common conditions among SAS-B approvals include anxiety, cancer-related symptoms (e.g. pain, nausea, anorexia), epilepsy, insomnia, and spasticity in multiple sclerosis. CBD-only products are being used in all of these conditions, but there is a greater use of them in patients with epilepsy and anxiety.
The TGA has published a series of clinical guidance documents that summarise the available evidence for medicinal cannabis products in chronic pain, palliative care, epilepsy, spasticity in multiple sclerosis and chemotherapy-induced nausea and vomiting.
With dozens of clinical studies now underway, researchers continue to identify additional potential applications for medicinal cannabis.